BBC News, Nottingham
 BBC
BBC“It’s horrible having to tell customers that their life-changing medicine isn’t available any more.”
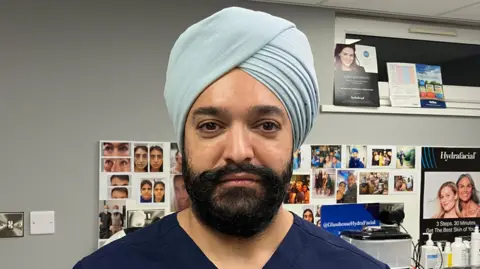
Harvinder Singh, a manager at Glasshouse Chemist in Nottingham, said it started experiencing stock shortages three years ago, and said this had fuelled customers’ anger over time.
He said morale was low among staff, and added: “I understand it, I truly feel for our customers because they just want to improve their health and I can’t help them.”
A survey published this month by the All-Party Parliamentary Group (APPG) on Pharmacy, a cross-party organisation, found medicine shortages were a “persistent and widespread issue”.
Medicines for attention deficit hyperactivity disorder (ADHD), epilepsy, blood pressure, as well as anti-depressant and hormone replacement therapy treatments were among the most affected, Harvinder said.
While many customers were understanding of the changes, others have become “irate and aggressive” towards staff, he said.
Harvinder added: “They say we’re incompetent, that we don’t know how to manage medicines, that our pharmacy is getting worse.”
The APPG on Pharmacy survey – of 112 pharmacists and team members – said 84% of pharmacists reported daily shortages, and another 14% experienced them several times a week.
In the survey, Labour MP Steve Race – chair of the APPG on Pharmacy – said action around shortages was “urgently needed”.

Harvinder explained staff often receive prescriptions that the pharmacy cannot supply due to shortages.
They would then have to contact the customer’s GP to find an alternative medicine.
These alternatives could have more side effects and be less effective, but Harvinder said “that’s all we can offer them”.
He said, as a result of this, his pharmacy now spent 14 extra hours a week trying to tackle the shortages.
“We don’t have time to take care with our customers and answer their questions and help them understand their medicines – it’s so limited now,” Harvinder added.
He said being a pharmacist was “disheartening” right now, and added he even discouraged his children from studying pharmacy at university.
“It feels like our profession is sinking – it’s not a nice place to be,” he added.
‘Too little too late’
Harvinder said Pharmacy First – the initiative that refers the public to community pharmacies for minor illnesses and repeat medicines before attending GP practices – had been a positive initiative.
He said the scheme brought in more funds and had helped take pressure away from GPs.
However, Harvinder is worried the initiative may be “too little too late”.
“We’ve expressed our concern, we’ve petitioned and seen no results,” he added.
“Our regulators have acknowledged that there is an issue but they have never given us a solution.”
Rebecca Dickenson, clinical pharmacy lead for the NHS Nottingham and Nottinghamshire integrated care board (ICB) – which oversees the city and county’s pharmacies – said: “Any abuse of pharmacy staff is unacceptable under any circumstances.
“Our community pharmacies will do everything they possibly can to support patients, but sometimes aren’t able to due to circumstances beyond their control.
“Medicine shortages are caused by national and sometimes global issues. Some medicines may not be available due to problems with manufacturing, transport, high demand, or issues sourcing the ingredients.”
She advised customers to only order medicines they need in good time, and try other pharmacies if they could not get it from their nominated chemist.
“It is important that you do ask for advice about next steps, as missing some medicines can cause harm and your prescriber may need to consider an alternative,” she added.




